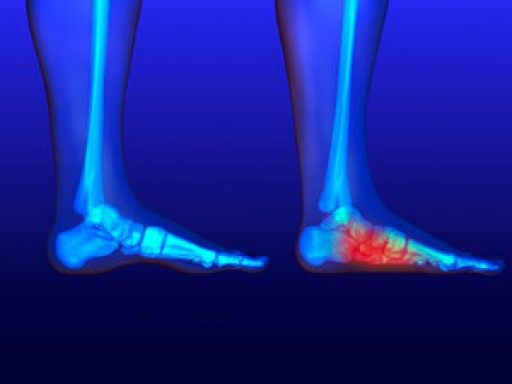
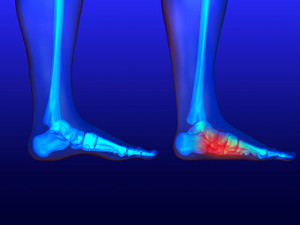
Fallen arches is a term used to describe flat feet that develop during adulthood. This is in contrast to flat feet that are present from early childhood, when the arch of the foot simply doesn’t form. Fallen arches, on the other hand, are not caused by the arch of the foot not developing, but rather by the arch forming and then collapsing over time. This is often due to weakening of the ligament that supports the arch. When the ligament loses its strength, it can no longer hold up the arch and the arch slowly lowers, creating a flat foot. Fallen arches can occur slowly due to the natural wear-and-tear caused by aging, or may be related to an injury. Another common cause is pregnancy, where hormones relax ligaments throughout the body, including those in the feet, which can lead to structural changes. Fallen arches can cause symptoms that range from mild discomfort to significant chronic pain. If you are experiencing foot pain, please consult with a podiatrist.
Flatfoot is a condition many people suffer from. If you have flat feet, contact one of our podiatrists from Foot Health Center of Merrimack Valley. Our doctors will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
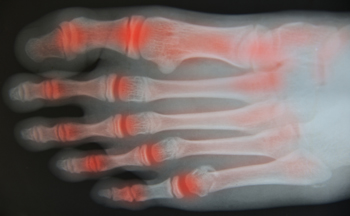
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
- Pain around the heel or arch area
- Trouble standing on the tip toe
- Swelling around the inside of the ankle
- Flat look to one or both feet
- Having your shoes feel uneven when worn
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions please feel free to contact one of our offices located in North Andover, and Tewksbury, MA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.